Mammography: What You Need to Know
Mammography is a type of medical imaging that uses low-energy X-rays to examine the breast for diagnosis and screening of breast diseases, such as breast cancer. It is one of the most effective ways to detect breast cancer early, when it is most treatable. In this blog post, I will explain what mammography is, how it works, what to expect, and what the results mean.
What is Mammography?
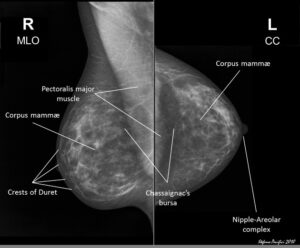
Mammography is a procedure that involves placing the breast on a special X-ray machine and taking images from different angles. The images are then analyzed by a radiologist, who is a doctor specialized in interpreting medical images, for any signs of abnormality. Mammography can be used for two purposes: screening and diagnosis.
Screening mammography is done for women who have no symptoms or problems with their breasts. It is recommended by various health organizations as a routine test for women of certain age groups, usually starting from 40 or 50 years old. The goal of screening mammography is to find breast cancer early, before it causes any symptoms or spreads to other parts of the body.
Diagnostic mammography is done for women who have symptoms or problems with their breasts, such as a lump, pain, nipple discharge, or changes in the shape or size of the breast. It is also done for women who have an abnormal finding on a screening mammogram or a physical exam. The goal of diagnostic mammography is to confirm or rule out the presence of breast cancer or other breast diseases.
There are different types of mammography machines that use different technologies to create the images. The most common types are:
- Digital mammography: This type of mammography uses electronic sensors to convert X-rays into digital images that can be stored and viewed on a computer. Digital mammography has some advantages over film mammography, such as lower radiation dose, better image quality, and easier image manipulation and transmission.
- 3D mammography: This type of mammography, also known as breast tomosynthesis or DBT, uses a rotating X-ray tube to take multiple images of the breast from different angles. These images are then reconstructed into a three-dimensional image set that can be viewed as thin slices of the breast. 3D mammography has some advantages over 2D mammography, such as better detection of small cancers, fewer false positives, and less need for additional tests.
- Contrast-enhanced mammography: This type of mammography uses an injection of a contrast agent, which is a substance that makes blood vessels more visible on X-rays. The contrast agent helps highlight areas of increased blood flow in the breast, which may indicate the presence of cancer. Contrast-enhanced mammography has some advantages over conventional mammography, such as better visualization of lesions, especially in dense breasts.
How Does Mammography Work?
Mammography works by using X-rays, which are a form of electromagnetic radiation that can penetrate through tissues and create images based on the different absorption rates of different tissues. X-rays are produced by an X-ray tube that emits a beam of electrons that hit a metal target (usually tungsten) and generate X-rays. The X-rays then pass through a filter (usually aluminum) that removes the low-energy X-rays that are not useful for imaging. The filtered X-rays then reach the breast, where they are partially absorbed by the tissues and partially transmitted to the detector. The detector can be either a film cassette or a digital sensor that converts the X-rays into an image.
The image quality and radiation dose of mammography depend on several factors, such as:
- The voltage (kVp) and current (mA) of the X-ray tube: These determine the energy and intensity of the X-rays produced by the tube. Higher voltage and current produce higher-energy and higher-intensity X-rays, which can penetrate deeper into the tissues and create sharper images. However, they also increase the radiation dose to the patient and the risk of radiation-induced damage to the tissues.
- The exposure time (s) and number of exposures: These determine how long and how many times the X-ray beam is turned on during the procedure. Longer exposure time and more exposures produce more images and more information for diagnosis. However, they also increase the radiation dose to the patient and the risk of radiation-induced damage to the tissues.
- The compression force (N) and thickness (cm) of the breast: These determine how much the breast is flattened and spread out during the procedure. More compression force and thinner breast reduce the overlap of tissues and create clearer images. However, they also increase the discomfort and pain for the patient during the procedure.
- The type and size of the detector: These determine how well the detector captures and converts the X-rays into an image. Larger detectors cover more area and produce larger images. Digital detectors have higher resolution and sensitivity than film detectors and produce sharper images.
The radiation dose of mammography is measured in milligray (mGy), which is a unit of absorbed dose that indicates how much energy is deposited in the tissues by the X-rays. The average radiation dose of mammography is about 4 mGy per breast, which is equivalent to about 0.4 mSv of effective dose, which is a unit of equivalent dose that indicates the potential biological effect of the radiation on the tissues. The average background radiation dose that people receive from natural sources (such as cosmic rays and radon gas) is about 3 mSv per year. Therefore, the radiation dose of mammography is comparable to about two months of background radiation exposure.
The risk of radiation-induced cancer from mammography is very low, but not zero. It is estimated that for every 100,000 women who have annual screening mammograms from age 40 to 74, about 125 will develop radiation-induced breast cancer and about 16 will die from it. However, this risk is outweighed by the benefit of early detection and treatment of breast cancer, which can save thousands of lives. The risk of radiation-induced cancer also depends on several factors, such as:
- The age of the patient: Younger patients have more sensitive tissues and longer life expectancy, which increase the risk of radiation-induced cancer.
- The frequency and duration of screening: More frequent and longer screening increase the cumulative radiation dose and the risk of radiation-induced cancer.
- The type and quality of mammography: Different types and qualities of mammography have different radiation doses and image qualities, which affect the risk of radiation-induced cancer and the accuracy of diagnosis.
What to Expect?
Mammography is a simple and safe procedure that usually takes about 15 to 30 minutes to complete. Before the procedure, you will be asked to:
- Inform the doctor or technologist if you are pregnant or breastfeeding, as mammography may not be suitable for you or may require special precautions.
- Inform the doctor or technologist if you have any breast symptoms or problems, such as a lump, pain, nipple discharge, or changes in the shape or size of the breast.
- Inform the doctor or technologist if you have any medical conditions or allergies, especially if you are allergic to contrast agents or iodine.
- Inform the doctor or technologist if you have any previous mammograms or other breast imaging tests done at another facility, and bring them with you if possible, as they may help with comparison and interpretation.
- Remove any jewelry or metal objects from your upper body, as they may interfere with the X-rays.
- Wear a two-piece outfit that allows easy access to your breasts, such as a blouse and skirt or pants.
- Avoid using any deodorant, talcum powder, lotion, perfume, or cream on your underarms or breasts on the day of the procedure, as they may show up on the images and cause confusion.
During the procedure, you will be asked to:
- Undress from the waist up and put on a gown that opens in the front.
- Stand in front of the mammography machine and place one breast at a time on a flat plastic plate.
- Hold still while another plastic plate presses down on your breast and compresses it firmly for a few seconds. You may feel some discomfort or pain during this step, but it is necessary to spread out the tissues and obtain clear images. You can ask the technologist to adjust the compression force if it is too uncomfortable for you.
- Breathe normally while the X-ray tube moves around your breast and takes images from different angles. You may hear some clicking or buzzing sounds during this step.
- Repeat the same steps for your other breast.
After the procedure, you will be asked to:
- Wait for a few minutes while the technologist checks the quality of the images. You may need to repeat some images if they are blurry or incomplete.
- Dress up and resume your normal activities. You may experience some soreness or swelling in your breasts for a few hours after the procedure, but this is normal and will subside soon. You can apply a cold compress or take a pain reliever if needed.
- Follow up with your doctor or radiologist for your results. You will usually receive your results within a few days by mail, phone, or online portal. If you have any questions or concerns about your results, do not hesitate to contact your doctor or radiologist.
https://coverstoryexpress.com/breast-cancer-awareness-month-more-than-just-pink-ribbons/
What Do The Results Mean?
The results of mammography are reported using a standardized system called Breast Imaging Reporting and Data System (BI-RADS), which assigns a category number from 0 to 6 based on the findings and recommendations. The categories are:
- Category 0: Incomplete – This means that additional imaging or information is needed before a final assessment can be made. You will be asked to return for more tests, such as additional mammograms, ultrasound, MRI, or biopsy.
- Category 1: Negative – This means that there are no signs of cancer or other abnormalities in your breasts.